Anesthesia in Rwanda – a learner’s perspective
 A month in Kigali has flown by, and I am already thinking about when I can go back. Through my transitional internship program, I had the chance to observe the practice of anesthesia in Rwanda and see the educational collaboration of CASIEF & HRH with the University of Rwanda first hand. There are 4 referral-level, teaching hospitals of Rwanda, 3 in Kigali, and another in Huye (Butare) in the southern part of the country, a 3.5 hour drive from Kigali. While most of my time was spent at CHUK – the largest public hospital in the country, I also visited King Faisal – a private hospital, and the Rwandan Military Hospital, each with its unique atmospheres.
A month in Kigali has flown by, and I am already thinking about when I can go back. Through my transitional internship program, I had the chance to observe the practice of anesthesia in Rwanda and see the educational collaboration of CASIEF & HRH with the University of Rwanda first hand. There are 4 referral-level, teaching hospitals of Rwanda, 3 in Kigali, and another in Huye (Butare) in the southern part of the country, a 3.5 hour drive from Kigali. While most of my time was spent at CHUK – the largest public hospital in the country, I also visited King Faisal – a private hospital, and the Rwandan Military Hospital, each with its unique atmospheres.
The affiliated medical school at The University of Rwanda has its own residency program, which started in the mid 2000’s. Enrollment has been steadily increasing, more exponentially since about 2011, and today there are 30 residents total divided among the 3 years. In Rwanda, after graduating medical school (which is 6 years, immediately after high school), one is required to do 1-2 years of general practice, working as a family medicine physician in a rural district hospital, often as the sole provider. Only after completing this can one then apply for specialty training. For anesthesia, this consists of 3 clinical anesthesia years, much like in the States. (Next year, the training program will be extended to 4 years; concurrently, there is some talk of doing away with the mandatory service prior to specialty training.)

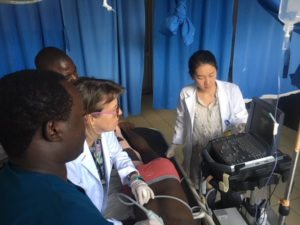
Each Monday all the residents from all 4 hospital sites convene at CHUK for didactics, led by the CASIEF & HRH volunteer anesthesiologists. The residents are split into Foundations (CA-1’s) and Core (CA-2’s and CA-3’s) for small group sessions in the morning, followed by a case presentation and other interactive lessons in the afternoon, often related to simulation or ultrasound. When I was there, the residents were prepping for their end of the year exams, so they were all eager to hone down core concepts. For me, this month was an excellent introduction to anesthesia and I found it very helpful learning with the Foundations group. The rest of the week, I would spend time in the operating rooms and the intensive care unit, where I was paired with a CA-3 Rwandan resident. At CHUK, there is one attending, with one to two senior residents (but usually only one) overseeing the 6 main operating rooms, each of which has a CA-1 or non-physician anesthetist (NPA, equivalent of a CRNA in the US) assigned. There was a separate team of residents for the 2 operating rooms in the maternity ward.
The breadth of cases in the main OR was quite impressive: all kinds of pediatrics (and only one peds surgeon), neurosurgery and orthopedics (mostly trauma, including late presenting trauma), urology, gastrointestinal/general, and ENT. While I had visited district and referral hospitals in other sub-Saharan countries, these in Kigali were much more advanced and well-equipped. It was a refreshing experience seeing the successful delivery of a relatively higher level of medical care. There were a several interesting and difficult airway cases, including a child with a large laryngeal papilloma, who ultimately needed an emergent tracheostomy after multiple failed intubations; luckily, communication was excellent among all the teams, and the ENT surgeon was already scrubbed and standing by while we were trying to get the airway.
There is one communal tea room, where everyone (nurses, doctors, technicians, cleaning staff, etc.) can mingle and grab a cup of tea or snack when there is down time. The next case would start…whenever it would start. That could range from 15 minutes to 1hr+ depending on the presence of the proper personnel, equipment, or the patient.

At King Faisal, I spent most of my time in the ICU. This hospital is well-equipped and privately funded. You talk to any non-medical expatriate living in Kigali and this is the hospital they will know. Many of the doctors are foreign-trained. I happened to be there the day of multidisciplinary ICU grand rounds. We all stood in a large circle in the ICU – about 30 people including anesthesia, surgery, internal medicine, and ENT residents (that particular day’s case was about a goiter). It was led by a neurosurgery attending, so his residents were there as well. There was even a cardiology attending (one of twelve cardiologists in the country!). The neurosurgeon posed clinical questions about the case and went around the circle asking each of the residents. No powerpoint slideshow or paper handouts, just good old fashioned verbal communication.
During my last week, I also visited the Rwandan Military Hospital, and was struck by their military-speed efficiency. While the first case began an hour after its designated start time (not uncommon in Rwanda), the room turnover for the subsequent cases was done with lightning speed. Just when the first patient settled and stabilized in the PACU, it was time to bring in the next one. I was also expecting the patients to be mostly older men, but this hospital actually serves the general public as well, and they do all kinds of cases including pediatrics and OB.
Being a PGY-1 was a challenging yet exciting experience. Most foreign residents visiting Rwanda were there to teach and offer their clinical expertise. There’s a bit of an expectation of any ‘mzungu’ at the hospital that you are there to impart your wisdom and help improve current practices. While I was comfortable adjusting an insulin regimen or diuresing someone with CHF after 10 months doing mostly internal medicine rotations, I had very little experience as an anesthesia provider. It was a preview of all the exciting things ahead, and a humbling reminder that I was about to embark on ‘intern year 2.0’. Still, some interesting differences in practice have stuck with me, like the regular use of halothane or just funny semantics like calling it propoket rather than ketofol. Overall, this month got me super pumped to know that I am finally about to start learning and practicing my chosen specialty.

Another thing I was impressed by was the strength and organization of the residency program and the collaboration with CASIEF/HRH. Each year, two Rwandan residents are chosen to rotate at hospitals in the US and Canada, all with the support (including financial) of the University of Rwanda and the Ministry of Health. Anesthesiology is becoming a more and more popular specialty choice in Rwanda, I think in part due to this strong partnership. The profession grew from only one anesthesiologist in the entire country after the genocide in 1994 to over ten new anesthesiologists minted each year, with many pursuing subspecialty training as well. The current group of residents are part of the new wave of anesthesiologists, and have the insight and numbers to direct what their field will look like. They are bright and see the unique position they are in. Down the line, the plan is to wind down foreign support so there can be a permanently self-sustaining training program in Rwanda. I am optimistic it will be a success.
Yuanting Zha
Incoming CA-1 resident at Brigham and Women’s Hospital in July 2018

